Pad the Shoulder
Bulking up the deltoid isn’t necessarily going to protect the shoulder. Keep the cuff strong and if you are going to “pad” up anything, make it your legs.
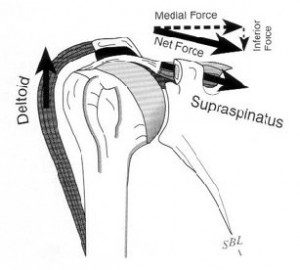
Bulking up the deltoid isn’t necessarily going to protect the shoulder. Keep the cuff strong and if you are going to “pad” up anything, make it your legs.

Studies continually show the benefits of conservative management of rotator cuff tears versus operative treatment. Many patients are having surgery when they could easily benefit from PT alone, at a fraction of the cost.
Lenny Macrina demonstrates manual therapy techniques to restore motion and reduce injuries in baseball pitchers.

Lenny Macrina, Director of Physical Therapy at Champion PT and Performance, discusses 3 ways to improve the overhead position.