Restoring Shoulder Soft Tissue Mobility in Baseball Pitchers
Lenny Macrina demonstrates manual therapy techniques to restore motion and reduce injuries in baseball pitchers.
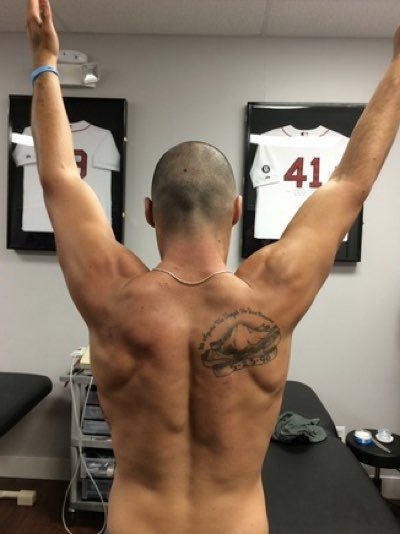
Lenny Macrina demonstrates manual therapy techniques to restore motion and reduce injuries in baseball pitchers.

Lenny Macrina, Director of Physical Therapy at Champion PT and Performance, discusses 3 ways to improve the overhead position.
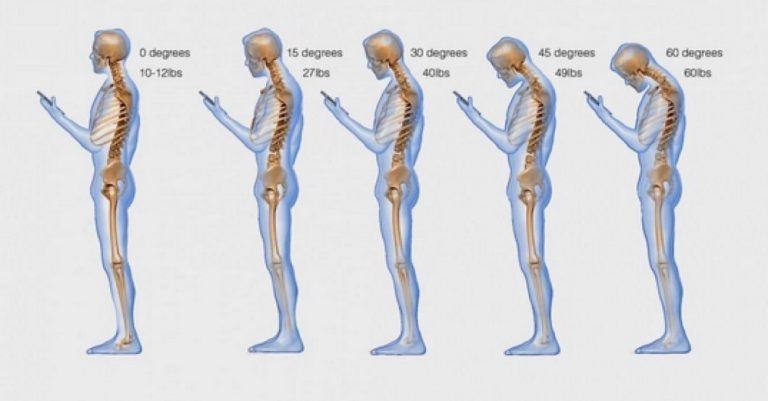
What if I told you that the you are doing something over a 100 times a day that is killing your posture, reducing your performance, and causing many issues like neck, back, and shoulder pain? Would you want to fix it? It may be easier than you think and help you more than you realize.

The most common complication following ACL reconstruction is loss of full motion, which can result in poor outcomes and satisfaction. Avoiding loss of motion is key by performing appropriate rehabilitation. Here are 3 ways to avoid loss of knee extension.